THE AUSTRALIAN FINANCIAL REVIEW MAGAZINE
Modern medicine has had its way for too long. Microbes are our predators, and they’re starting strike back.
By Wilson da Silva
THERE ARE three enormous cedars just beyond the entrance to Fairfield Hospital. Single-storey redbrick buildings follow, their white-painted trimmings shining in the sun. Manicured lawns surround them, skirted by clusters of agapanthus and African daisies, stands of sugar gums, wattle trees and silver birch. The smell of freshly-cut grass pervades, occasionally ruffled by passing nurses in pressed white cotton and sensible shoes, their voices mixing with the buzz of a whipper snipper nearby and the “tick, tick, tick” of a sprinkler.
The road is some distance away and no traffic can be heard. A little further down the hill and to the south-west, past the golf course and the picnic areas, the Yarra River snakes its circuitous way towards the glass and steel of the Melbourne skyline.
It seems safe, tranquil. A bit like Sunday in suburbia. It’s hard to believe this is also the edge of darkness.
For this is where Australia’s first and last line of defence is on standby for war. Here stands the National High Security Quarantine Laboratory, Australia’s only top-level human ‘hot lab’ capable of dealing with the deadliest of diseases. Inside, the airlocks are in working order, disposable protective suits sit neatly stacked in their cabinets and the incubators continuously heat and reheat.
It is a war room ready for a conflict scientists hope will never be fought. Yet in their hearts, they know it is only a matter of time.
Early battles are already raging: sporadic viral skirmishes in pockets of the developing world such as Zaire, or new drug-resistant infections establishing beachheads in major cities like New York. Infectious diseases are returning with a potency never seen before. Scientists are already calling the 1990s the Post Antibiotic Age.

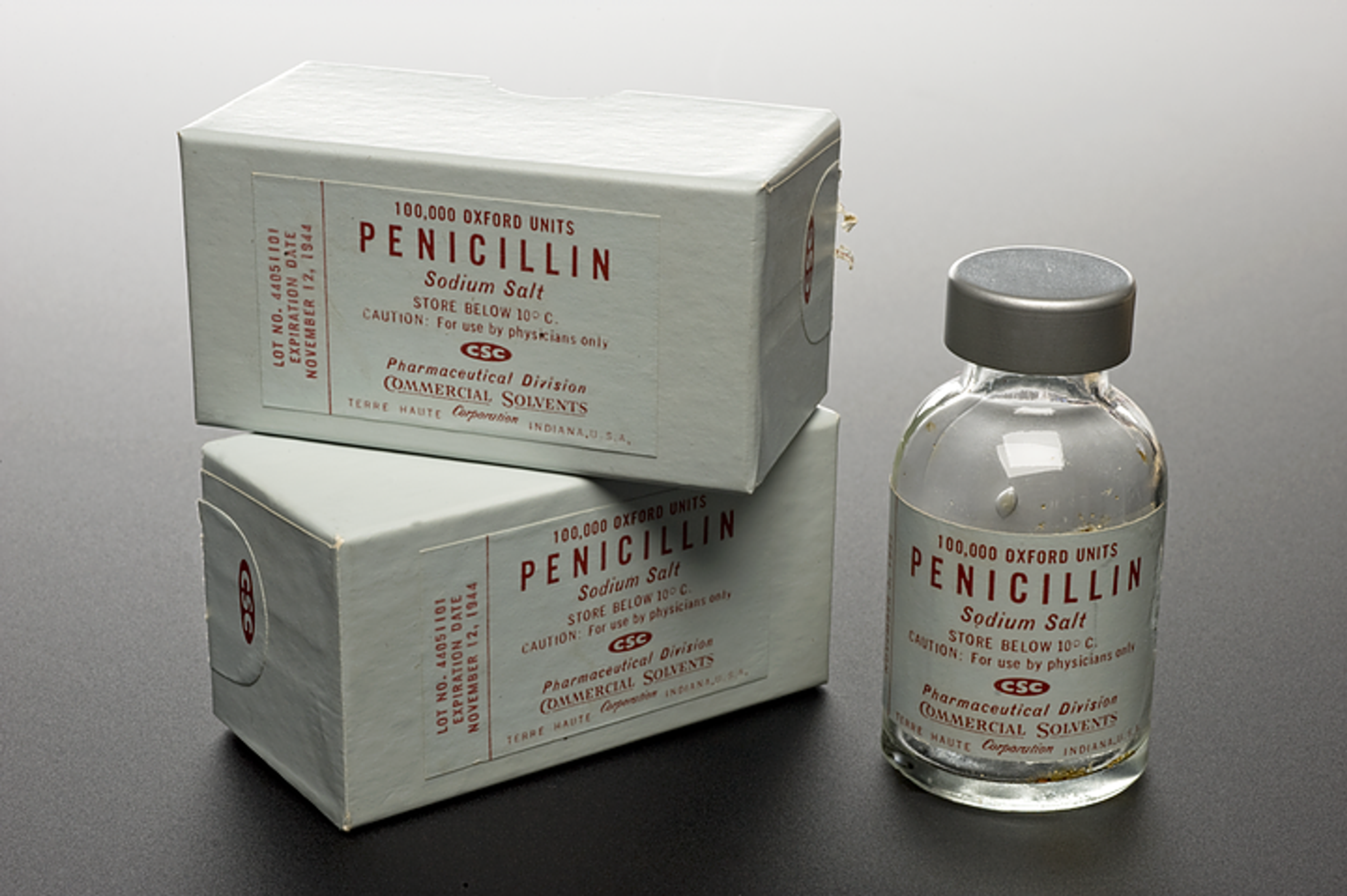
SINCE PENICILLIN appeared in 1944, we have grown blasé about microbes. As diseases reeled and retreated, our confidence grew into arrogance, an arrogance typified by U.S. Surgeon-General William H. Stewart, who announced in 1969, “The war against infectious diseases has been won.” Medical experts then turned their attention to chronic disease – a mind-set that has prevailed.
Until now. The medical world has been feeling a lot less smug lately. Hospital wards are filling with patients harbouring new strains of micro-organisms causing old diseases that are now extraordinarily difficult to cure: tuberculosis, cholera, malaria, pneumonia, dengue fever, gonorrhoea, even the golden staph bacillus. Meanwhile, new diseases and conditions have emerged: Ebola, hantaviruses, Lyme disease, Legionnaire’s disease, AIDS, toxic shock syndrome ... the list goes on.
“Despite historical projections to the contrary, we remain vulnerable to a wide array of new and resurgent infectious diseases,” said Dr David Satcher, director of the Centres for Disease Control (CDC) in Atlanta, in a 1994 report to U.S. President Bill Clinton. “Our anti-microbial drugs have become less effective against many infectious agents. At the same time, our ability to detect, contain and prevent emerging infectious diseases is in jeopardy.
“Drugs that once seemed invincible are losing their effectiveness,” he warned. “Increased microbial resistance has resulted in prolonged hospitalisations and higher death rates from infections [and] has required much more expensive – and often more toxic – drugs or drug combinations, even for common infections.”
Dr Satcher is not the only one who is worried. The World Health Organisation recently brought together experts from 23 countries to discuss drug resistance. A WHO conference on 'emerging viruses' is planned for early next year.
The Ebola epidemic in Zaire, coupled with the Dustin Hoffman film Outbreak and the recent best-seller, The Hot Zone (both based on the deadly virus) have raised fears of a doomsday virus. More recently, The Coming Plague – a new book in which science journalist Laurie Garrett details an avalanche of deadly diseases already descending on humanity – is walking off the shelves in the United States.

Scientists agree things don’t look good; some say they are actually worse than the Hollywood hype. Microbes appear to be evolving and mutating faster than before – and faster than researchers can invent new drugs. So many new variants are being found that it appears “there has been a change in the microbial world”, according to John Montagne, director of the National Institute of Allergy and Infectious Diseases at the U.S. National Institutes of Health. He told a press conference in Atlanta in July that researchers are reporting faster mutations among pathogens as disparate as those which cause malaria and influenza.
American Nobel laureate Dr Joshua Lederberg summed up the problem at a New York forum last year: “We’re running out of bullets for dealing with a number of these infections. Patients are dying because, in many cases, we no longer have antibiotics that work.”
Evolutionary theorist George Williams, of the State University of New York, argues this is merely Darwinism at play. Driven by 20th century technology and human activity, evolution is generating new pathogenic abilities to outwit our medical defences.“Bacteria can evolve as much in a day as we can in 1,000 years,” he says in his new co-authored book, Evolution and Healing. “We cannot evolve fast enough to escape from micro-organisms.”
It’s this kind of development that is troubling Dr Michael Catton, medical virologist at the Victorian Infectious Diseases Reference Laboratory, which runs the high-security 'hot lab'. “The likelihood is that new things will appear, or that old things will come back to haunt us and we will be poorly equipped to face them,” he says. “My fear is we won’t be sufficiently organised to respond to new threats. It’s increasingly looking like a very, very worrying scenario.”

CATTON IS A 35-YEAR-OLD virologist from New Zealand. Like most of his counterparts today, he was born into an age when the medical school dictum was “Antibiotics Rule OK”; a world where science had, it seemed, won the upper hand. There were no wards filled with children dying of pneumonia, meningitis or typhoid; scarlet fever, diphtheria and rheumatic fever were diseases of the Dark Ages. While doctors in the 1940s treated them regularly, their counterparts today would hardly recognise the symptoms.
They may soon have a chance to learn, thanks to rising drug resistance. When an antibiotic is used, most bacteria are killed off, leaving only the mutants that can outlive the drug. With no competition for food, the mutants breed prodigiously. Next time antibiotics are used, the weaker ones die, leaving the strongest mutants to multiply. In this way, drug resistance is 'bred' into each generation of micro-organisms.
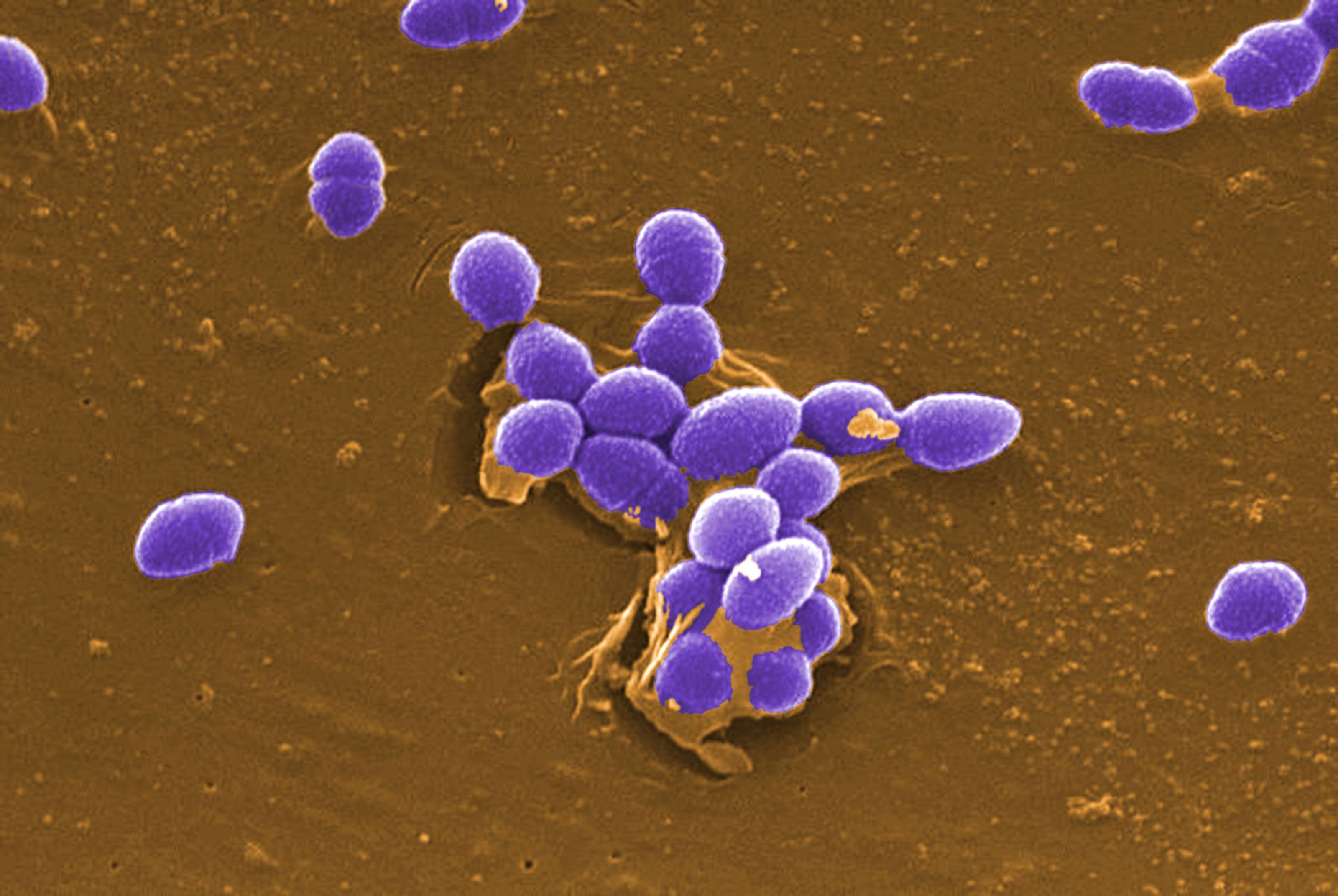
Take penicillin: in 1952, infection-causing Staphylococcus bacteria were almost completely susceptible and the scourge became an irritant. By 1982, 90 per cent of Staphylococcus strains were resistant. New antibiotics were developed, but new resistance has arisen – and much more quickly than expected. Today, about 40 per cent of hospital staphylococci infections are resistant to every antibiotic but one – Vancomycin, the most expensive and toxic. Doctors now try drug after drug and some patients die before the right mix is found.
“The only thing you can do is try to contain it. There’s no vaccine, no drug that has the slightest effect on it.”
Geoffrey Cannon, author of Superbug: Nature’s Revenge, blames doctors for handing out antibiotics as if they were lollies. “Fifty thousand tonnes of antibiotics are being used every year on humans and animals,” he writes. “This is literally a colossal overkill. Antibiotics now do more harm than good.”
Environmental disturbance is helping flush out the new nasties. Humans are trekking into rarely-visited ecological niches like rainforests, rubbing shoulders with exotic animals or conducting other activities, like logging and dam building, that unbalance local environments. Reforestation in Connecticut saw an explosion in deer tick numbers, some carrying the bacterium that is now known to cause Lyme disease.
Identified in 1975, this new – which causes severe arthritis, lethargy and brain disorders – has now been detected in Europe and some scientists say it is present in Australian ticks. Land clearing in South America brought people close to rodents carrying the virus that causes Junin haemorrhagic fever, triggering deadly epidemics.
The outbreak in Zaire of the Ebola virus - thought to reside in primates - is the most recent example. A forestry worker infected hospital staff in the city of Kikwit and by May the disease had spread to three other towns. Crack medical teams flew in while a panicked government mobilised troops to surround infected areas. The WHO has put the death toll at 233 so far (with another 63 people recovering) and expects complete containment within months.
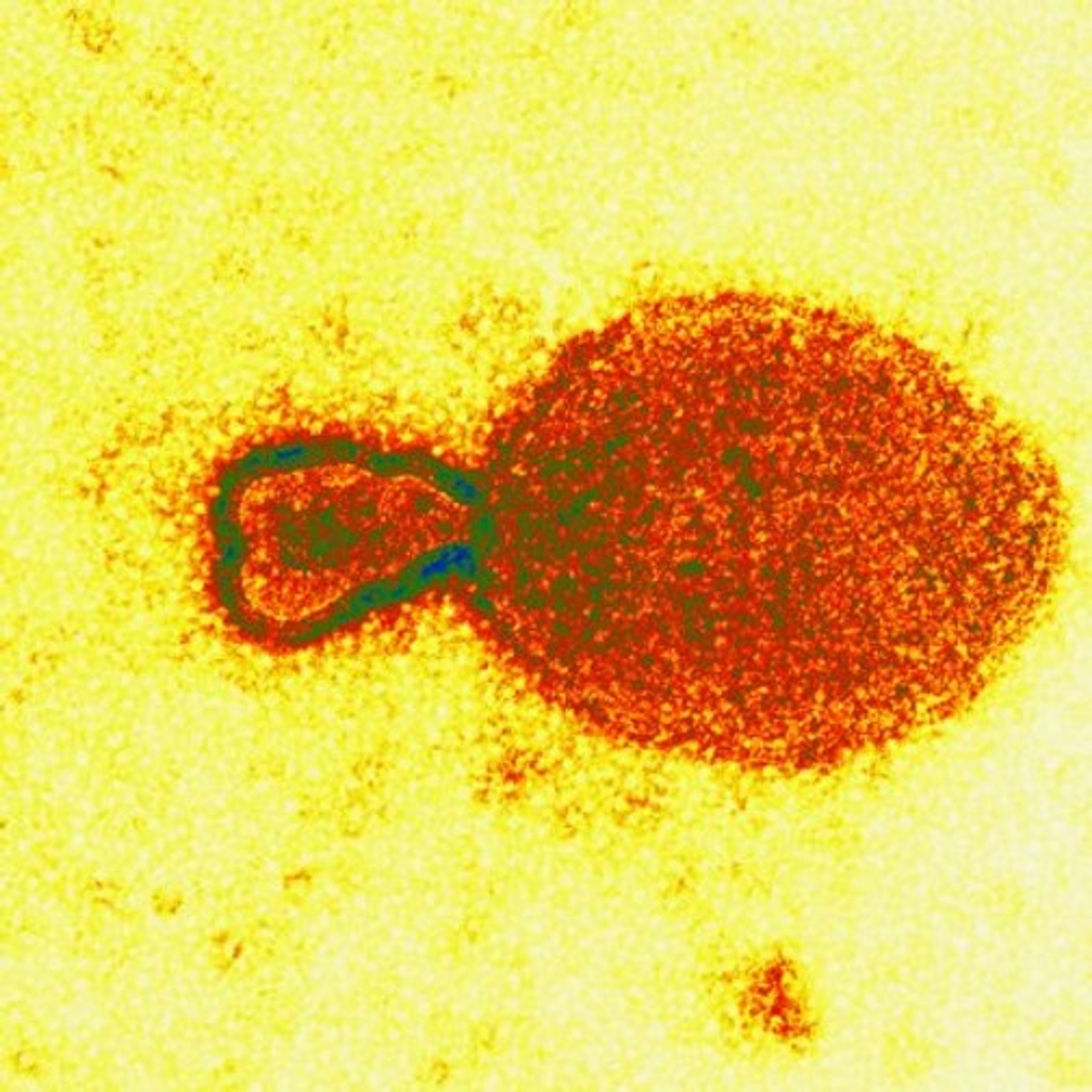
Of the emerging viruses identified so far, Ebola is the most feared. Discovered in 1977, it triggers high fever, bleeding gums and vomiting of blood. Organs haemorrhage profusely and victims bleed from every orifice. An agonising few days later, eight out of 10 victims are dead, their insides liquefied.
“The only thing you can do is try to contain it,” says Professor Frank Fenner, an internationally renowned virologist at the John Curtin School of Medical Research in Canberra. “There’s no vaccine, no drug that has the slightest effect on it.”
Scientists say the chances of a global outbreak are small: the disease is transmitted by body fluids and the infected fall ill and die before they can travel far. There was only one known case outside Zaire this time and it set off a panic: a scientist in Britain studying a sample accidentally jabbed his thumb with a syringe. He developed haemorrhagic fever and was isolated for 49 days; the hospital was emptied of patients and the large medical staff treating him was quarantined. The laboratory where he worked was shut down, its employees put under surveillance and the scientist’s friends and family restricted to their homes. He recovered and there were no other cases.
In two previous epidemics, 1976 and 1979, Ebola killed over 400 in Zaire and Sudan before burning out. An outbreak at an American research facility in Virginia in 1989 was triggered by an infected Asian monkey; scores of the creatures died and a number of lab workers also became ill. Luckily, this strain was not lethal to humans.

Ebola is a filovirus, a type of organism seen only once before: in 1967, when lab staff in Marburg, Germany, fell violently ill after handling Ugandan monkeys. Named after the town, this first recorded outbreak hospitalised 31 and killed seven. There have been only three known cases since.
“We never know when it will break out and where,” says Dr Sheth Musoke, a Kenyan who contracted Marburg from a patient in 1980 but recovered. “When it comes, it never really gives us time to play around with the virus. And in between the outbreaks we cannot do much.”
Researchers have found little-understood variants of Ebola, which may be transmissible through the air, in Asia: antibodies discovered in monkeys from Indonesia and the Philippines and in the blood of Filipino workers on Luzon and villagers and macaques on Mindanao. No one knows if there is a link between the Ebola variants in Asia and African Ebola, nor where the virus resides between outbreaks. While the American outbreak suggests the Asian variants are not fatal to humans, scientists do not know for certain.
Other recent pathogens on the “Very Deadly” list are arenaviruses: Junfn, Sabia, Lassa and hantaviruses are some examples, with the latter being of most concern.
Researchers have traced hantaviruses, first identified in 1977, back to the Korean War, when more than 2,500 United Nations troops contracted a strain of the mystery disease and hundreds died. Now known to inhabit rodents living in an ecological niche near the Demilitarised Zone, it has since appeared in the US where, in 1993, it caused an outbreak in New Mexico that killed 44 of the 80 Navajo Indians infected. Sufferers developed cramps, high fever, extreme breathing difficulty and kidney failure.
Since the disease was identified, outbreaks have been tracked in Greece and the Balkans; milder forms found in Scandinavia, large areas of the former Soviet Union and in parts of Europe. In South Korea, 13 per cent of rats in Seoul carried antibodies to the virus and a global study has since found such rat antibodies in other parts of Asia, South America and Australia.
A variant has been found in 80 per cent of rats in Baltimore, USA, and scientists speculate the virus may partly be responsible for the high level of kidney disease among inner-city Baltimore residents, some of whom have also tested positive for hantaviruses. In May this year, a teenage boy in Texas died within hours of being hospitalised for an infection; the following month, authorities announced the virus was present in five per cent of the State’s rodents. U.S. authorities now expect 50 to 100 cases a year.
Another bug to strike fear recently is streptococcus group A, thought to be a recently-emerged mutant. Related to an otherwise humdrum microbe, this is the 'flesh-eating' bacteria that made headlines in Britain last year, causing 'necrotising fasciitis' – melting muscle and fat. U.S. officials estimate it has killed 450 Americans each year from 1989 to 1991 and infects between 10,000 and 15,000 annually; its virulence appears to be increasing.
Last year, local scientists came across Australia’s own emerging virus, the world’s newest: Equine morbillivirus. A previously unknown organism, it appeared without warning near Brisbane, killed 14 horses and hospitalised two men. One, a stablehand, recovered after two months; the other, horse trainer Vic Rail, died a ghastly, wheezing death, his lungs ravaged.
While scientists are unsure where Equine morbillivirus originates, they admit they were extremely lucky this time. “Once it’s in your body, it’s extremely virulent. Really virulent,” says Dr Allan Gould, a molecular biologist at the Australian Animal Health Laboratory in Geelong, whose genetic sequencing pinned down the culprit. “The thing that stopped this from being a major catastrophe is the fact that it’s not very contagious.”
HIV is the best-known emerging virus. The WHO estimates 19.5 million people have been infected since the disease was first recognised in 1981. At the start of the year, more than 1 million had developed full-blown AIDS, a 20 per cent increase on 1994. Asia, until recently free of the scourge, has seen HIV spread at breakneck speed; about 2.5 million people in the region are infected. In India, the WHO estimates 1.6 million infections; the virus is so new there that fewer than 1,000 have developed full blown AIDS.
While scientists are unsure where Equine morbillivirus originates, they admit they were extremely lucky this time. “Once it’s in your body, it’s extremely virulent. Really virulent,” says Dr Allan Gould, a molecular biologist at the Australian Animal Health Laboratory in Geelong, whose genetic sequencing pinned down the culprit. “The thing that stopped this from being a major catastrophe is the fact that it’s not very contagious.”
HIV is the best-known emerging virus. The WHO estimates 19.5 million people have been infected since the disease was first recognised in 1981. At the start of the year, more than 1 million had developed full-blown AIDS, a 20 per cent increase on 1994. Asia, until recently free of the scourge, has seen HIV spread at breakneck speed; about 2.5 million people in the region are infected. In India, the WHO estimates 1.6 million infections; the virus is so new there that fewer than 1,000 have developed full blown AIDS.
THE 1990s ARE A PARADISE for infectious diseases. Not just for the ones that are tasting hunans for the first time, but also for the old faithfuls. There have been two dengue fever epidemics centred on Townsville since 1992, with the last affecting 663 people. Dengue also broke out in Britain earlier this year, infecting 800; tyres imported into the U.S. brought dengue-laden mosquito larvae, triggering another outbreak. Two years ago, the WHO declared tuberculosis a global emergency: the age-old disease, now resistant t o a number of drugs, is killing more than 2.5 million people a year and likely to kill 4 million annually by 2005. In 20 of the 27 countries of central and eastern Europe and the former Soviet Union, TB is roaring back.
In the US, the sharp rise in TB cases in 1985 caught everyone by surprise. There are now 26,000 cases annually and epidemiologists estimate 10 million to 15 million Americans are infected and likely to develop TB in the future. A form of TB resistant to all drugs surfaced in HIV patients in New York some years back; it has since spread across the state’s health system. Medical staff nursing HIV patients grew sick and died, at times before stumped doctors could identify the cause. Tuberculosis now requires more toxic and more expensive drugs and longer stays in hospital. In the U.S., treatment can cost US$17,000 a person; for multi-drug-resistance, costs can soar to US$350,000 a patient.
Large populations have helped disease, too: the more hosts, the more mutations microbes undergo. They therefore love the big smoke and there’s never been more of that than in the 1990s. A century ago, 15 per cent of the world’s population inhabited cities; today, nearly half live there.
And it is the 'mega-cities' of the developing world – which can least afford civil and public health infrastructure – that top the list. Of the 14 cities with populations of 10 million or more, only four are in the industrialised world. By 2015, according to the World Bank, there will be 21 such cities, only three located in rich countries.

Modern food production has also assisted the spread of infections. Mechanisation and distribution has allowed products with a biological origin to be processed and shipped more efficiently and for lower cost. But it has also amplified accidental contaminations; a pathogen that escapes screening can merge with a large batch of final product and contaminate the whole. In 1993, meat contaminated by a new and nasty strain of Escherichia coli bacteria, known as O157:H7E, was supplied to a U.S. hamburger chain. Thousands of customers developed bloody diarrhoea and kidney dysfunction and four children died.
Modern human behaviour at the end of the 20th century is also abetting the bugs: more wars and civil strife than ever before, a perceived increase in sexual activity, intravenous drug use and a burgeoning but untraceable trade in sex tourism.
“The historical processes that have given rise to the emergence of new infections throughout history ... are accelerating,” says Stephen Morse, a Rockefeller University professor considered a leader in emerging diseases. “Humans are not powerless against this relentless march of microbes. The primary problem is no longer virological, but social.”
Once a nasty bug comes to light, it is only a plane ride from being a global phenomenon. Air travel has grown 17-fold since the 1950s: more than 1 billion passengers fly every year, and more than 300 million of them cross national borders.
Travel is blamed for the global spread of drug-resistant cholera. From 1991 to 1994, more than a million cases and nearly 10,000 deaths were reported in the Americas, the first epidemics there for almost a century. Whereas for most of human history populations were isolated and diseases evolving in one area stayed there, allowing locals to develop some resistance, today anywhere is just hours away from anywhere else.
Dr Lederberg, the microbiologist Nobel laureate, is succinct: “The microbe that felled one child in a distant continent yesterday can reach yours today and seed a global pandemic tomorrow.”
Ironically, the outbreak just about every expert fears is a variant of a bug we know well: influenza. Not your garden variety, though, but a truly nasty killer that arises infrequently from radical mutations.
nfluenza is one of the fastest chameleons of the microbial world. Every year it evolves new strains, and every year our immune systems eventually overcome them. Still, each year the virus kills 1,500 in Australia and between 10,000 and 45,000 in the U.S.
Occasionally, the virus undergoes segmental shift, a radical mutation. Most of these have little or no effect. But sometimes the mutations create 'pandemic influenza', strains so potent that they kill even the healthiest.
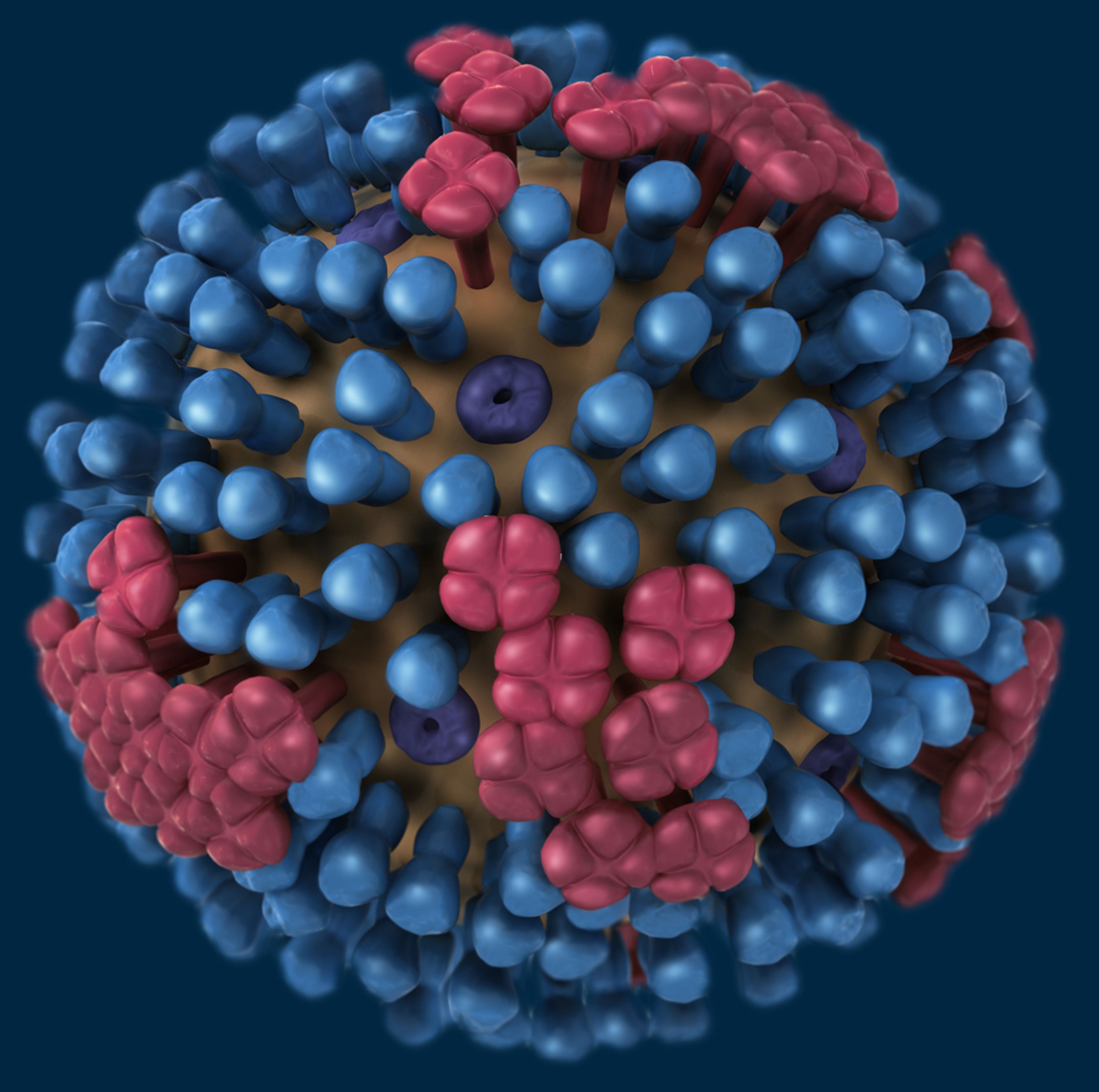
The most deadly pandemic recorded was the so-called Spanish flu. In 1918-19 it spread across the world in eight months and killed at least 20 million. Less deadly pandemic strains have followed: 'Asian flu' in 1957-58 killed some 2.8 million and the 'Hong Kong flu' of 1968-69 killed 1.4 million. A smaller outbreak in 1977 affected only people under 27 years of age and was genetically identical to the 1957 strain; this led researchers to surmise that the strain had broken out of laboratory deep freeze and spread, but had little success with those old enough to have developed a previous immunity.
Scientists even know where the pandemic will start: China. Recent studies suggest the country is the global source for almost all pandemic flu, thanks to centuries of integrated farming of pigs and ducks. Ducks are major reservoirs of flu virus, and pigs the mixing sites for different strains. Gene segments from two strains are therefore brought together regularly, re-assorting to produce a new virus that can infect humans. Occasionally, the resulting strain is super-deadly.

AT A U.S. CONGRESSIONAL hearing in 1981, the-then head of the U.S. National Institutes of Health, Dr Richard Krause, was asked why so many diseases were emerging. “Nothing new has happened,” he said “Plagues are as certain as death and taxes.”
Although we think of micro-organisms as lowly, they are in fact our only true predators. “We’re in eternal competition,” Dr Lederberg told a meeting of American investment bankers last year. “We’re not alone at the top of the food chain.”
When the plagues come, they will have been aided by government cutbacks in public health measures. Whether due to budgetary pressure in rich countries or the need to repay loans in poorer nations, governments looking for savings have been targeting infectious disease programs in the mistaken belief that the scourge was on the wane. Cutbacks were the main cause for the resurgence of tuberculosis in the U.S. and for new epidemics of diphtheria in Russia, where there have been more than 10,000 cases since 1993 thanks to falling levels of immunisation.
Garrett in her book quotes a 1993 finding that of the 34 labs designed to warn of global outbreaks, half could not isolate yellow fever and more than half failed tests for Japanese or California encephalitis; most could not detect hantavirus and few had the reagents to test for Ebola, Marburg or Lassa viruses. Another study found that after two decades of belt-tightening, health departments of most American states were run by, at best, a skeleton staff.
In 1986, just as the comeback of tuberculosis was kicking in, the multi-drug-resistance unit at the CDC was closed. All told, cuts in TB programs during the 1980s saved the U.S. about $280 million. In the five years to 1994, the country spent more than $1.4 billion annually on multi-drug-resistant tuberculosis, according to The Economist magazine.
“The CDC’s programs for dealing with infectious diseases have been nibbled to death by inflation,” says Dr Frederick Murphy, a former director of the CDC and the first man to see Ebola under the microscope. “The budgets are the same in today’s dollars as they were 12 years ago. In effect, these programs have lost half of their purchasing power, while at the same time we’ve seen an explosion in AIDS and other infectious diseases.”
The decay of public infrastructure has also allowed previously contained micro-organisms to proliferate, even in rich countries. A breakdown of water-filtration systems in the American city of Milwaukee in 1993 led to more than 400,000 people being infected with Cryptosporidium (a diarrhoea-causing waterborne parasite) and 4,400 people were hospitalised.

Scientists are agitating for change. Prof Jonathan Mann of Harvard University, a former chief of the WHO’s AIDS program and an outspoken voice on infectious diseases, has been leading a cabal of medicos urging the creation of a global monitoring system capable of reacting to emerging microbial crises.
Mann fears the world’s next pandemic may be circulating now, spreading without our knowledge, just as HIV did: “The conditions of the modern world are uniquely favourable to the rapid global spread of infectious diseases. A global health approach is needed now to detect as rapidly as possible the next inevitable infectious disease pandemic.”
The WHO has approved a modest program to upgrade the world’s dated medical reporting network, but cannot find the US$2.5 million needed. A bolder plan to establish a worldwide string of laboratories with improved surveillance and training is being pushed by the CDC, estimated to cost US$175 million a year. But this is thought too ambitious by member nations, who expect the U.N. agency to safeguard the health of 5 billion people with a budget the size of a large metropolitan U.S. hospital. The WHO’s budget for emergency infectious outbreaks is US$35,000.
Medical experts fear it will take a truly nasty global outbreak to stir governments into decisive action: an outbreak as widespread as AIDS but more visible and immediate, such as of Ebola or hantavirus. Until then, we wait for the plague bomb to explode.

At the Victorian Infectious Diseases Reference Laboratory, 'hot lab' microbiologist Marie Gerard walks through the dimly lit corridors to a tall and heavy looking locker. The door swings open slowly; inside there is shelf after shelf of glass vials caked over in frost and kept at -70˚C. Dry ice vapour rolls downward as she pulls one of the small boxes out and holds it for me to see.
“Have a look,” she says, holding up the samples kept by the quarantine scientists for reference. A thousand different diseases rest in a frozen miniature museum. Among them are samples taken from the men who fell ill to Australia’s own deadly emerging disease, Equine morbillivirus.
There is only a moment’s peek before the extreme cold forces her to replace the vial and close the cryogenic locker.
Tick, tick, tick.
